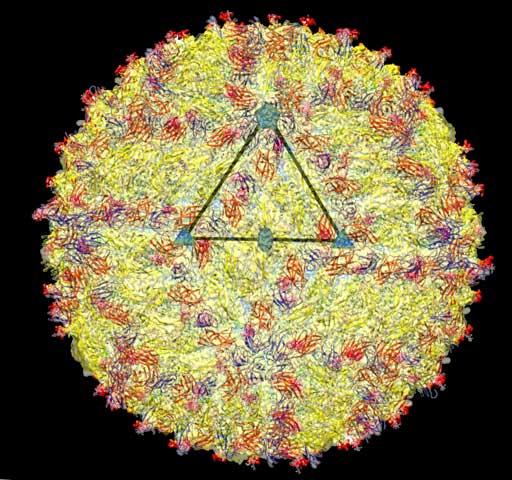
A cryo-electron microscopy image of the Zika virus structure. Researchers at Washington University in St. Louis (WashU) have established the first models of Zika virus transmission from a pregnant mouse to her fetus. The infected mice, described May 11 in Cell, demonstrate Zika virus invasion and damage to the placenta, and then infection of the mouse fetus, leading to many of the same conditions observed in human infants. The new mouse models can also be used as a tool to develop treatments or vaccines.
"There have been questions regarding whether in utero transmission of Zika virus actually causes disease in the fetus. While the evidence has been mounting, our data confirms that Zika virus can cause congenital problems, including fetal death," says Michael Diamond, a viral immunologist at WashU.
Creating even a general mouse model of Zika virus infection has been a challenge because mice aren't normally susceptible to the virus. To get around the animals' immune defenses and study viral transmission during pregnancy, Diamond and his colleagues, including post-doctoral fellow Jonathan Miner, developed two models. In one, the female mice were genetically wired to have a defective immune system, creating a model of severe disease when infected with Zika. In the second model, the female mice were genetically normal, but received injections of an antibody that partially prevented their immune systems from functioning.
When the genetically immunocompromised mice became pregnant and were infected with Zika virus, the researchers--including Indira Mysorekar, a reproductive biologist at WashU and co-senior author on the study, and her postdoctoral fellow, Bin Cao--were able to observe the viral transmission to the mouse fetus. They found that Zika preferentially infected the placenta: viral levels there were 1,000 times higher than they were in the mother's serum.
Once in the placenta, the virus infected the trophoblast cells and injured the fetal blood capillaries. Previous work has demonstrated that late-stage placental cells were resistant to Zika infection, but these mouse models show that the virus is able to cross the barrier between the maternal tissue and the fetus earlier in pregnancy.
In many of the genetically immunocompromised pregnant mice that were infected, the fetuses died before being born. Those that survived to term were markedly smaller and had Zika virus replicating in their brains and central nervous system.
"Most of the time, the placenta is an effective barrier between the mother and her fetus," says Mysorekar. "But Zika is able to overcome it and progressively infect different trophoblast layers. We see the virus in the fetal blood vessel lining and then in circulation, and soon after, we see that it's able to go to the brain."
The researchers are continuing to study the two mouse models to determine how Zika breaches the placental barrier and what further consequences there may be for infected mouse pups. "The two models provide different aspects of the biology," explains Diamond. "In the knockout model, we see the growth retardation, fetal demise, and injury to the brain. In the blocking-antibody model, which is less severe, we can follow the development of the mice after birth. We plan to test them for any developmental changes that a milder Zika virus infection could have caused."
Source: Cell Press
 Print Article
Print Article Mail to a Friend
Mail to a Friend
